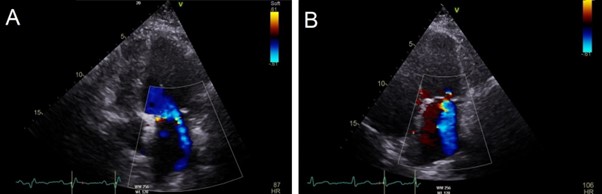
Introduction: Cardiac implantable electronic device (CIED) diagnostics are of significant clinical utility when managing the heart failure (HF) population. This report highlights a novel service in which cardiac physiologists act autonomously upon CIED diagnostics to identify and manage patients at risk of decompensated HF.
Patient presentation: A 71-year-old female with ischaemic heart disease and paroxysmal atrial fibrillation (AF) presented via a remote CIED transmission. The device diagnostics indicated possible decompensated HF and therefore initiated a telephone triage. The telephone review of the patient’s symptoms outlined worsening dyspnoea of recent onset and reduced capacity to perform daily activities. An urgent appointment in the physiologist-led clinic was made for a face-to-face clinical assessment.
Initial work up: the physiologist assessment identified bi-basal crepitations, bilateral pitting oedema, a pansystolic murmur and HF symptoms correlating with the onset of AF. Suspecting decompensated HF, an ECG, echocardiogram and blood test were performed within the physiologist service.
Diagnosis and management: 12-lead ECG: The 12-lead ECG showed AF with rapid ventricular response and confirmed the diagnosis of persistent AF highlighted within device diagnostics. The addition of an echocardiogram and blood test were clinically useful in confirming an acute HF exacerbation.
Echocardiogram: prior to presentation, the patient had documented mild mitral regurgitation (MR) and short paroxysms of AF. At the time of clinical assessment, this had worsened to moderate MR. The exacerbation of the existing MR was attributed to the onset of persistent AF with poor rate control. Imaging using transthoracic echocardiogram confirmed the finding of a pansystolic murmur outlined in the physiologist clinical assessment.
Bloods: urgent blood tests confirmed an elevated NT-pro BNP of 628 pg/ml.
The patient received a same-day review by our electrophysiology consultant who supported the physiologist diagnosis of decompensated HF in the context of persistent AF. A medical review of the patient’s prescription resulted in a change from carvedilol to bisoprolol and initiation of oral furosemide. The patient was also listed for an urgent pulmonary vein isolation (PVI).
PVI: 4 weeks after the patient was identified to be at risk of an acute HF decompensation through the physiologist-led service, they underwent a successful PVI. This success was initially short lived, with 1.5 days in sinus rhythm post procedure before re-initiation of AF. However, this episode of AF persisted for 1 month before terminating back to sinus rhythm, which has remained ever since.
A repeat clinical assessment performed 6 weeks post-intervention demonstrated no HF signs or reoccurrence of AF.
Conclusion: A physiologist-led HF management service can streamline the time from patient presentation to HF review, potentially reducing the risk of HF hospitalization and improving patient outcomes. Given the appropriate training, physiologists can identify and clinically assess patients at risk of worsening HF and highlight these patients to the necessary services for further management. ❑
Figure 1: CIED diagnostics outlining increased HeartLogic Heart Failure Index correlating with onset of persistent AF
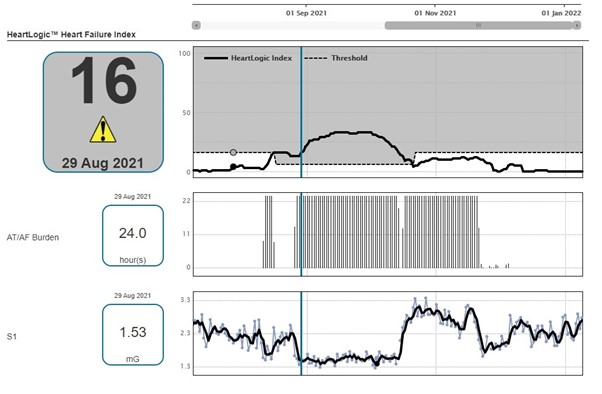
Figure 2: Transthoracic echocardiogram images taken in the apical 4-chamber view highlighting mild MR pre-presentation (A) and moderate MR at the time of presentation (B)