Background and objectives: Cardiac resynchronization therapy (CRT) using bi-ventricular pacing is class I recommendation for symptomatic patients with heart failure (LVEF ≤35%), QRS duration ≥150 msec and LBBB QRS morphology. Left bundle branch area pacing (LBBAP) has been reported as an alternative option for CRT. The aim of this study was to assess the feasibility and outcomes of LBBAP in patients eligible for CRT.
Methods: Patients with CRT indications were subjected to LBBAP. Peri-procedural outcomes & QRS duration were recorded. Changes in New York Heart Association (NYHA) class, need for HF hospitalization, echocardiographic data, lead-device parameters were evaluated at follow-up. HF status was assessed by clinical (no HF hospitalization and improvement in NYHA class) and echocardiographic response (≥5% improvement in LVEF).
Results: LBBAP was attempted in 16 patients (mean age 59.3 ± 7.04 years, 37.5% women, ischaemic cardiomyopathy in 33.3%). All patients had baseline LBBB. Pacing threshold and R-wave amplitudes were 0.8 ± 0.3 V at 0.5 ms and 12.1 ± 3.5 Mv at implantation and remained stable during mean follow-up of 11.25 ± 3.7 (range 6–18) months. LBBAP resulted in significant QRS narrowing from 147.5 ± 9.7 to 116 ± 10.2 ms (p<0.01). LVEF improved from 28.2 ± 2.8% to 38.9 ± 5.1% (p<0.01). Clinical and echocardiographic improvement was observed in 77% and 74% of patients, respectively.
Conclusion: LBBAP is feasible, safe and provides an alternative option for CRT. LBBAP provides low and stable pacing thresholds and is associated with improved clinical and echocardiographic outcomes. ❑
Figure 1: Changes in QRS duration and ejection fraction at follow up
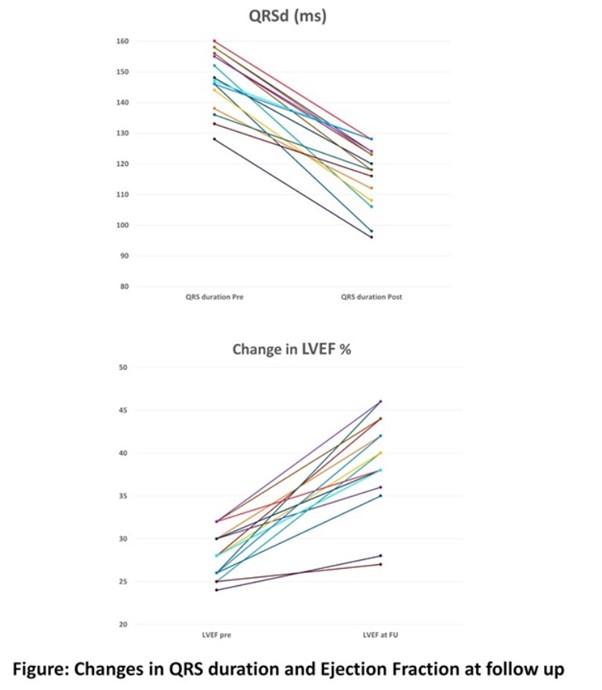
Table 1: Baseline, procedural and outcome characteristics
















