Introduction: With advances in cardiac resynchronisation therapy (CRT) equipment and operator experience, implant success is increasing. However, the commonest cause for procedural failure remains a lack of suitable pacing site due to an absent or insufficiently sized target vein. The role of computed tomography (CT) prior to CRT remains investigational, but improved imaging techniques allow assessment of target veins and access site patency. This may improve decision making for high-risk procedures.
Objectives: We sought to describe and assess the impact of CT prior to CRT upgrade/revision.
Methods: CT and fluoroscopic images were analysed for patients referred for CT prior to CRT upgrade/revision between 2015 and 2022 (Siemens SOMATOM Definition Flash 128-Slice Dual-Source CT Scanner and Siemens Syngo.via software) (Figure 1). Data obtained were: target vein identification on CT, target vein used at implant, subclavian vein patency, radiation dose and incidental findings.
Results: A total of 34 patients had CT prior to CRT upgrade/revision, mean age 73 years, 76% male. Reasons for upgrade were pacing-induced cardiomyopathy and/or deterioration of pre-existing cardiomyopathy (n=32), or LV lead displacement (n=2). Overall, 31 patients subsequently attended the lab. Subclavian vein patency was graded as patent, significantly stenosed or occluded with both CT and on-table venography (for patients attending the lab). There was 87% agreement between the two modalities. However, differentiating between stenosis and occlusion on CT is difficult. As such, these two findings were treated interchangeably for pre-procedure planning. If stenosis/occlusion are taken together the agreement between modalities is 98%. A suitable calibre posterior or lateral target vein was identified on CT in 32/34 cases (92%). Subclavian access was achieved in 27/31 patients attending the lab. In 26/27 cases (96%), CT accurately delineated cardiac vein anatomy. In 25/27 cases (92%) the target vein identified on CT was utilised. In one of the remaining cases, tight angulation prevented use of the CT-identified target; a small antero-lateral vein was used instead, though only three poles of a quadripolar lead were placed. In the second case, the target vein was occluded proximally and filled by small antegrade collaterals; an inferior bridging vein was used instead. Two patients did not proceed to upgrade partly due to poor targets on CT (small-calibre veins and/or suboptimal location); one declined given additional uncertainties of success, and the other was unsuitable for prolonged procedures due to advanced heart failure, which later required transfer for transplant assessment.
Mean CT radiation dose was 1426 mGy/cm. Median procedure radiation dose was 10192 mGy/cm2. Four patients had significant incidental findings: three had a left atrial thrombus, requiring changes to anticoagulation, and one patient had a lung nodule, requiring follow-up imaging.
Conclusion: Cardiac CT prior to CRT upgrade/revision enhanced pre-procedural decision making and supported changes in patient management in this small cohort. CT accurately identified target veins. Assessing subclavian venous patency was more difficult, though there was still high concordance between CT and on-table venography. The CT radiation dose is high relative to other cardiac CT, due to the addition of detailed subclavian imaging. Subsequent adaptation of the CT protocol has reduced radiation dose, whilst still allowing assessment of subclavian anatomy and patency. ❑
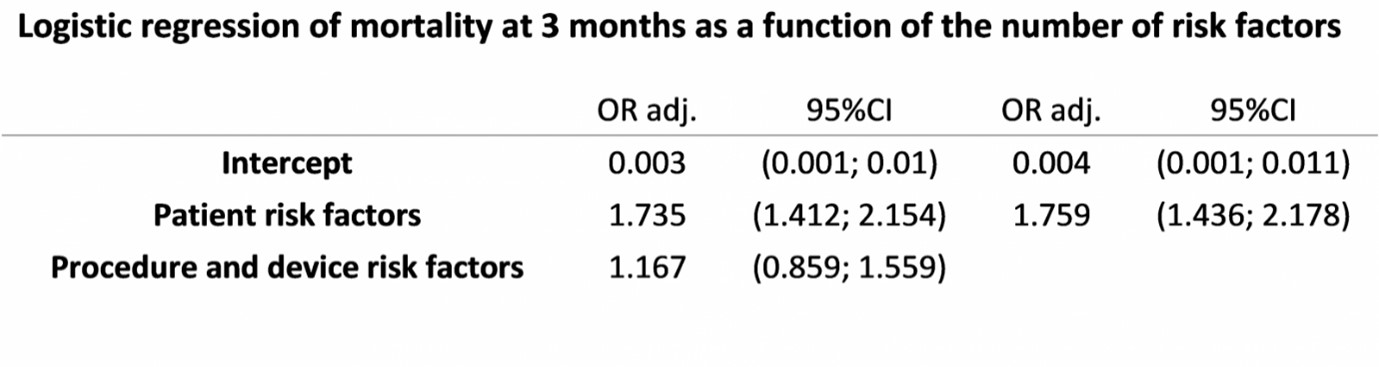
Table 1: Logistic regression of mortality at 3 months as a function of the number of risk factors