Introduction: Technological innovations, catalyzed by the COVID-19 pandemic, have opened new avenues for remote monitoring, screening and diagnostics in cardiovascular care. Atrial fibrillation (AF) has a huge healthcare burden within our health service and is a major contributor to presentations to health services, hospitalizations, morbidity and mortality. We identified an opportunity to digitize and enhance our pre-existing AF care pathways through the same day emergency care unit (SDEC) and through implementation of an early supported discharge pathway, using an approach that leverages digital remote monitoring technologies. In this abstract, we share our experience and the impact of our approach on clinical outcomes to date.
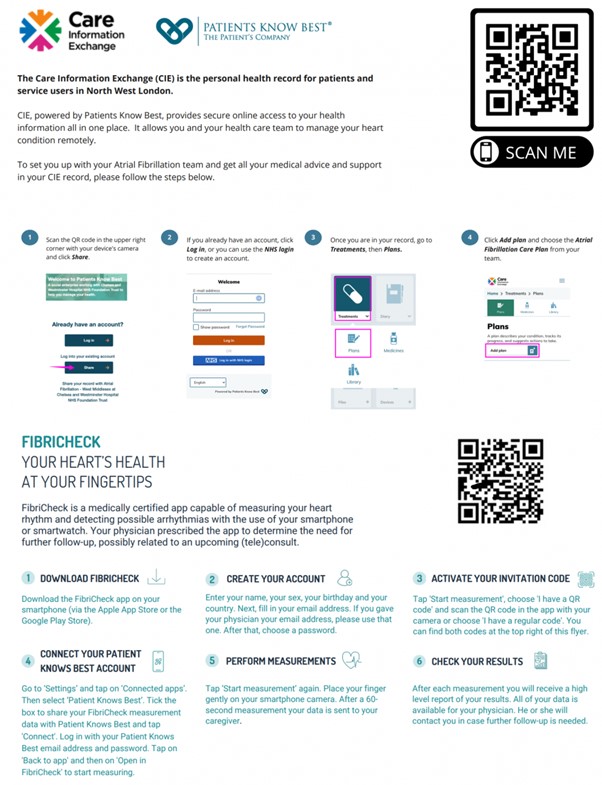
Methods: We conducted an initial audit of patients presenting to ED or admitted with newly diagnosed or poorly controlled AF, spanning a 6-month period from March to September 2022. We found that around 10% of patients reattended ED within 30 days of discharge with an arrhythmia-related presentation, of whom over a third required admission, representing an average of 5.5 bed days. With this in mind, we devised a digital model of care to enable patients to be remotely monitored for up to 2 weeks in their home environment while recovering from an acute hospitalization, aiming to reduce unplanned ED reattendances and readmissions, and to promote early supported discharge in suitable patients. Our approach integrated two digital elements: a smartphone-based heart rhythm and symptom monitoring app (FibriCheck) and a digital interface, integrated with the patient electronic health record, to which real-time device data can be uploaded and reviewed (Care Information Exchange/Patient Knows Best). A central sector-level remote monitoring hub, staffed by trained specialist nurses, managed the virtual AF ward environment and conducted telephone triage assessments, escalating to the cardiology team where needed. A traffic light system was employed, guided by NICE and ESC guidance, to determine parameters for care escalation, such as expedited review in SDEC or recommendations to attend ED for assessment.
Results: The pathway went live in November 2022 and we have enrolled 39 patients to date, 95% of whom engaged with remote monitoring. Six patients (15%) were appropriately advised to attend ED and a further 5 patients (13%) were instructed to attend for an expedited review in SDEC in view of abnormal parameters and/or symptoms following telephone assessment. Over a 3-month period, only 2 patients were hospitalized for an arrhythmia-related presentation (1 patient was non-compliant with remote monitoring, 1 patient ran out of bisoprolol). AF patients with early-supported discharge via the pathway had an average 4-day shorter length of stay. We have received positive patient feedback overall.
Conclusion: We share our experience of a novel digital model of care for remote monitoring of AF following acute hospitalization. Our findings suggest improved care delivery, reduction in rates of rehospitalization, shorter inpatient stay and improved patient experience. A similar care model could be replicated across other NHS trusts. ❑
Figure 1: Patient flyers used as part of the patient onboarding process for the Care Information Exchange platform and FibriCheck app