Background: Catheter ablation (CA) of ventricular tachycardia (VT) reduces ICD therapies in patients with VT due to structural heart disease (SHD). A structured ablation pathway may guide pre-ablation optimization of antiarrhythmic drugs (AAD) and ICD programming. We aimed to investigate impact of an ablation pathway on VT ablation outcome.
Methods: The study recruited consecutive patients with SHD undergoing VT ablation before (Cohort 1, 2015–2020) and after (Cohort 2, 2020–2022) the introduction of a VT ablation pathway. Cohort 2 had beta-blocker up-titration following first anti-tachycardia pacing. After first ICD shock, patients were started on class III AADs. Patients with ischaemic cardiomyopathy (ICM) were offered CA. Patients with non-ICM (NICM) had CA after second ICD shock. Potential demographic and clinical predictors of hospitalization for VT or heart failure (HF) were assessed. Cox regression and Kaplan-Meier analyses were performed.
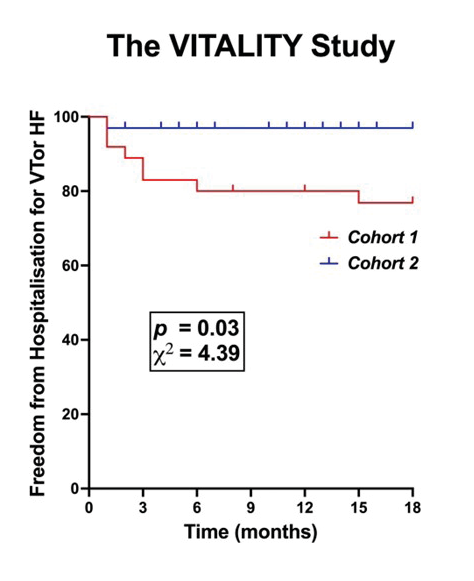
Results: Demographics were similar between Cohorts 1 and 2 (n=76 versus 43; age 60.5 ± 15.0 versus 59.3 ± 14.3 years; EF 39.2 ± 12.3% versus 38.5 ± 10.1%; NICM 57% versus 49%; PAAINESD 12.7 ± 6.5 versus 13.5 ± 7.1). Prior to CA, Cohort 2 received fewer ICD shocks (0.75 ± 0.87 versus 7.0 ± 8.9, p<0.01). Following ablation, fewer patients in Cohort 2 remained on ≥1 AAD (3.6% versus 42.5%, p<0.01), experienced VT (34.6% versus 51.4%, p<0.05) and ICD shocks (6.9% versus 21.6%, p<0.05). At 18 months, 93.5% of Cohort 2 versus 72.5% Cohort 1 were free of hospitalization from VT or heart failure (p<0.05). Cohort 2 (HR=0.01, p<0.05) and mappable VT (HR=0.31, p<0.05) independently predicts freedom from hospitalization for VT or HF.
Conclusion: Pre-ablation optimization of AAD and ICD programming through a VT ablation pathway improves VT ablation outcomes in patients with SHD. Future mechanistic studies to investigate upstream optimization of VT ablations are required. ❑
Figure 1