Background: Risk models have been utilised to predict major adverse events (MAEs) following transvenous lead extraction (TLE). We evaluated whether applying machine learning (ML-) techniques incorporating chest radiographs increased the ability of existing models to predict MAE (defined as procedure-related major complication and procedure-related deaths).
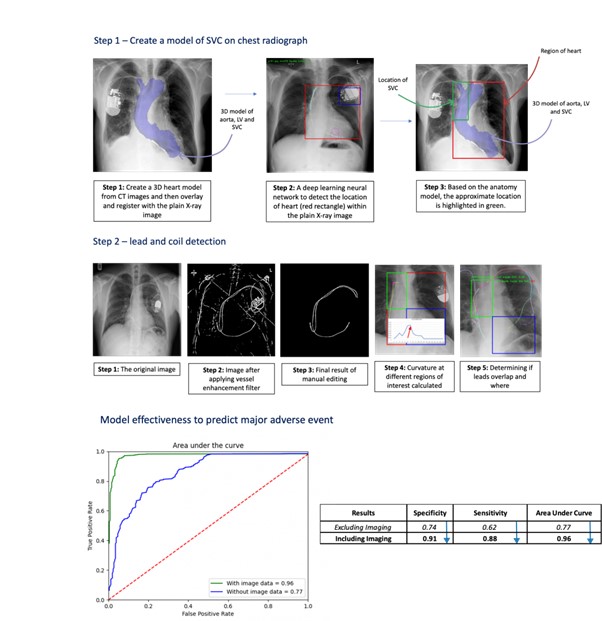
Methods: Two models were assessed whether ML would improve risk prediction compared to an existing risk score. Model 1: we designed and evaluated a ML-based risk model trained on the European ELECTRa registry of 3,555 patients undergoing TLE. This was tested on an independent registry of 1,171 patients undergoing TLE from our institution. This was compared with the published Electra Registry Outcome Score (EROS) – a risk score based on the ELECTRa registry. Pre-procedural demographic, clinical, device and lead variables were included. A self-normalising neural network (SNN), stepwise logistic regression, support vector machines (SVM) and random forest (RF) models were compared to the performance of EROS. Model 2: we integrated geometric features identified using artificial intelligence (AI) from a pre-procedure anterior posterior (AP) chest x-ray (CXR) into model 1. The method of identifying geometric features is illustrated in the figure. We evaluated if incorporating imaging data from a CXR could improve the model’s predictive capability.
Results: Model 1: there were 53 MAEs (1.7%) in the training cohort and 24 (2.4%) in the test cohort. Thirty-two clinically important features were used to train the models. ML techniques without incorporating radiographic imaging data were similar to EROS by balanced accuracy (stepwise logistic regression: 0.74 versus EROS: 0.70) and moderately superior by area under the curve (AUC) (SVM: 0.764 versus EROS: 0.677). Model 2: 1,050 cases out of the 1,171 patients at our institution had pre-extraction CXRs suitable for ML analysis. The computer vision algorithm was able to detect: i) the heart border: with 100% accuracy, ii) ICD coils: 98% accuracy, iii) acute angulation in the right ventricle (RV): 91% accuracy, iv) acute angulation in the superior vena cava (SVC): 70% accuracy. The following features correlated with MAEs: i) >50% of the ICD coil within the SVC, ii) >2 overlapping leads in the SVC, iii) acute RV lead angulation. Using these imaging features in the ML-model significantly improved prediction of MAEs: i) balanced accuracy from 0.74 to 0.91, ii) sensitivity from 0.62 to 0.88, iii) specificity from 0.73 to 0.90, and iv) AUC from 0.77 to 0.96.
Conclusion: Integration of imaging biomarkers from a plain AP CXR into risk prediction tools significantly increases the ability of ML models to predict risk of MAE following TLE. This may be integrated into heart team decision-making regarding extraction risk and resource allocation. Using these novel techniques in richer imaging data such as CT or fluoroscopy could provide more accurate ML- risk prediction models. ❑
Figure 1