Introduction: Leadless left ventricular (LV) endocardial pacing with the WiSE-CRT System (EBR Systems Inc) is a novel treatment in the field of cardiac resynchronization therapy (CRT). The system was designed to provide lateral wall LV pacing (LVP) in response to detection of a right ventricular pacing (RVP) stimulus from a co-implanted device. The result is biventricular pacing (BiVP) with the RV ahead roughly 30 milliseconds. Observational studies have reported the clinical efficacy of this treatment. However, it is unclear whether BiVP is the optimal pacing modality in these patients, particularly in the context of leadless left bundle branch area pacing (LBBAP), which is an emerging use for this technology.
Aim: We aimed to characterize the electro-anatomical activation patterns of patients receiving leadless CRT at different pacing modalities using electrocardiographic imaging (ECGi).
Methods: Eight patients treated with the WiSE-CRT system underwent an ECGi study. The following pacing modalities were tested: RVP; BiVP; LVP only; and LVP with an electrically optimized atrioventricular delay (AVD) in patients with sinus rhythm (SR). Reconstructed epicardial electrograms from ECGi were used to calculate LV activation time (LVAT-90), RV activation time (RVAT-90), BiV activation time (BIVAT-90), LV dyssynchrony index (LVDI), and BiV dyssynchrony index (BIVDI). For each metric, the percentage improvement compared to RVP was calculated.
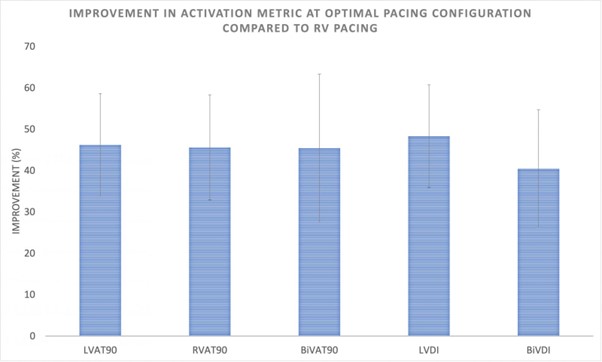
Results: Of the 8 patients, 5 were receiving LBBAP via LV septal endocardial pacing; the remaining 3 patients had received lateral wall LVP. The underlying rhythm in 4 patients was SR with left bundle branch block (LBBB), and atrial fibrillation (AF) with complete heart block (CHB) in the remaining 4. At the optimal pacing modality, leadless CRT achieved significant improvements in: LVAT-90 (46.2% ± 12.4, p<0.01); RVAT-90 (45.6% ± 12.7, p<0.01); BiVAT-90 (45.4% ± 17.9, p<0.01); BiVDI (40.3% ± 14.3, p<0.01) and LVDI (48.3% ± 17.9, p<0.01), see Figure 1. Overall, BiVP achieved significant improvements in BiVAT-90 (19.6% ± 12.8, p=0.02) and BiVDI (15.2 ± 12.6, p=0.05). The optimal pacing modality varied between patients. In patients with SR and LBBB, LVP with AVD optimization was the only pacing modality which was significantly superior to RVP (BiVAT-90 43.5% ± 11.7, p<0.01). In patients with AF and CHB, LVP was the optimal modality in 2 patients, with BiVP performing best in the remaining 2. BiVP achieved significant improvements in BiVAT-90 in patients with lateral wall LVP (39.4% ± 13.2, p=0.03), but not in those receiving septal LVP (7.8% ± 9.2, p=0.07), where LVP with or without AVD optimization was the best modality in 4 out of 5 patients.
Conclusion: Leadless CRT significantly reduces both electrical activation times and improves electrical dyssynchrony. Whilst BiVP did significantly improve BiV activation and dyssynchrony overall, it was the optimal pacing mode in only 2 patients. In patients with SR and LBBB, LVP with AVD optimization may improve BiV synchrony by allowing LV activation to fuse with native right bundle activation. In patients with septal WiSE-CRT implants, LV activation may be inhibited by a degree of apical septal refractoriness created by the early RVP wavefront. As such, individualized selection of the best pacing modality in each patient may be required with leadless CRT to accommodate for varying conduction disease phenotypes and implant locations. ❑
Figure 1: Improvement in activation metric at optimal pacing configuration compared to RV pacing