touchCARDIO coverage of data presented at ESC 2024
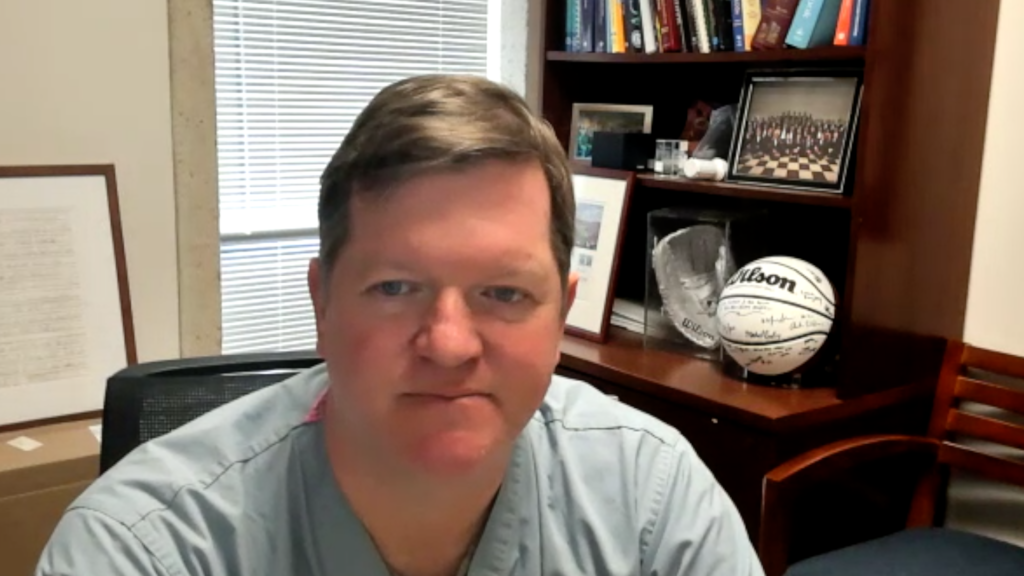
touchCARDIO spoke with Dr Mike Gibson, Harvard Medical School, Boston, MA, USA to discuss the results of his trial investigating the relationship between apolipoprotein A-I infusions and cardiovascular outcomes, presented at ESC 2024. He explains that while high-density lipoprotein (HDL) is generally associated with good outcomes, not all HDL is equally effective at removing cholesterol from plaque, a process known as cholesterol efflux, which is crucial for better outcomes after a heart attack.
Dr Gibson’s study involved infusing heart attack patients with CSL112, a form of apolipoprotein A, over a month and tracking their health for up to a year. The primary goal was to assess the 90-, 180 and 365-day rates of death, myocardial infarction (MI) and stroke, but results showed no significant difference between treated and control groups at 90 days. However, a notable reduction in total events was observed when multiple events were considered, particularly in patients with high baseline low-density lipoprotein (LDL) levels, who saw a 36% reduction in death, MI and stroke.
Dr Gibson suggests that future studies should focus on targeting the right patients—those with high LDL levels and significant plaque build-up—since they have more to gain from HDL infusion therapies. He concludes that the HDL hypothesis remains promising and warrants further investigation.
Disclosures: C Michael Gibson is a consultant for and has received grant/research support from CSL Behring.
This content has been developed independently by Touch Medical Media for touchCARDIO and is not affiliated with ESC. Unapproved products or unapproved uses of approved products may be discussed by the faculty; these situations may reflect the approval status in one or more jurisdictions. No endorsement of unapproved products or unapproved uses is either made or implied by mention of these products or uses by Touch Medical Media or any sponsor. Views expressed are the speaker’s own and do not necessarily reflect the views of Touch Medical Media.
Click here for more content on cardiovascular disease and for further ESC 2024 highlights visit here.
Transcript
Hi, I’m Mike Gibson, I’m an interventional cardiologist and professor of medicine at Harvard Medical School.
Q1. What is currently known about the association between apolipoprotein A-I infusions and cardiovascular outcomes?
Everyone knows that high HDL is associated with good outcomes.
The question is, if we raise people’s HDL, could we improve those outcomes? We failed a few times in the past, but the question is: “Did we just raise HDL, the number, or did we really improve the function of the HDL?”; “Was it really good cholesterol or maybe just, I don’t know, ‘meh’ cholesterol?”
HDL is made of apolipoprotein A, and there’s a way we measure just how good HDL is, and that’s called cholesterol efflux. What we know is this: not all HDL is created equally. Some HDL is better at ‘sucking’ the cholesterol out of your plaque. That’s called better cholesterol efflux. We also, importantly, know that those people after a heart attack who have good efflux, the ability to get the cholesterol out, they have better outcomes.
Q2. What were the aims, design and eligibility criteria of the study?
We know that good efflux improves outcomes, and what we have shown is that this CSL112 is an apolipoprotein A that we get from healthy human volunteers that works really well in terms of efflux.
What we did is we took heart attack patients, and we infused this apolipoprotein A, CSL112, four times over a month. And then we followed them out for 90 days and looked at death, heart attack and stroke. Then we also looked out at a 180 days and 365 days to see how they were doing.
Q3. What were the primary and secondary endpoints, and what results did you find?
The primary endpoint was the 90-day rate of death, MI, stroke. Secondary endpoints were 180 and 365 days. What we found was by 90 days there was no difference in the two strategies. Numerically, the curve started to diverge a bit between 90 days and a year, but again, did not achieve statistical significance.
But we got another question. The question was this: If we really look at multiple events, not just the first one, then we did see a reduction in the total number of events, because we’re looking at the burden of disease here.
And the second question we had: “How does your baseline LDL affect the results?”
And other studies have looked at a 100 as a cut[off] point, and we looked at people with an LDL above 100. And if you were hyperlipidaemic on entry, we did see a 36% reduction in death, MI, stroke. That was highly statistically significant.
If your LDL was well controlled, if it was 100 or less, there was no difference.
So, you know, HDL is the ‘garbage truck’. And if you have a lot of ‘garbage’, it makes sense to infuse HDL to get the garbage out. But if you don’t have a lot of garbage floating around, putting in huge numbers of garbage trucks didn’t help. So it all kind of makes sense.
Q4. What factors might have contributed to these findings?
I think if you’re hyperlipidaemic, you’ve got more plaque and you’ve got more of a target there to improve.
If you’re meeting the cholesterol guidelines and your LDL is quite low, there’s not as much of a target for improvement.
So, you know, we gotta give the right drug to the right patient at the right dose at the right time, and a patient has to have a viable target for improvement. In this in this case, it was having probably a lot of plaque.
Q5. On the basis of this, what are your recommendations for future study?
This was a big study: 18,200 patients. I think the HDL hypothesis – the idea that we can improve outcomes by improving the function, not the number, but the function of HDL – I think that hypothesis is still alive and kicking. It’ll be up to future researchers and ourselves to examine this further and see if we have other strategies replicate these results in the hyperlipidaemic patients.
Interviewer/Editor: Heather Hall
Cite: Gibson CM. Alipoprotein A-I infusions and cardiovascular outcomes. touchCARDIO, September 9 2024.