Heart failure (HF) is a complex syndrome caused by a variety of cardiac and non-cardiac diseases, and is associated with high mortality and hospitalization rates.1 Treatment has been traditionally based on a detailed history and physical examination. However, since cardiac biomarkers reflect the pathophysiology of HF, they add information to the clinical findings.1 The most widely used of these is natriuretic peptide (NP), which is helpful in the diagnosis and prognosis of HF. The management of HF is usually based on signs and symptoms (conventional care). Alternatively, the adjustments in medications can be made using biomarkers, in this case NPs. This strategy is referred to as ‘NP-guided therapy’, as shown in Figure 1. However, the superiority of this strategy over conventional care is not clear.1 This review summarizes the evidence for NP-guided therapy in patients with HF with either reduced or preserved ejection fraction (HFrEF and HFpEF), and also in patients hospitalized with acute HF.

Natriuretic peptide-guided therapy in heart failure with reduced ejection fraction
Treatment of patients with HFrEF has recently undergone a major therapeutic innovation with novel medical therapies, such as angiotensin receptor–neprilysin inhibitors, sodium–glucose co-transporter 2 inhibitors (SGLT2is) and soluble guanylate cyclase stimulators.2–5 These agents improve clinical outcomes and improve biomarkers closely related to the pathophysiology of HF. These biomarkers include: NPs, which are markers of myocardial stretch; cardiac troponin, a marker of myocardial damage; and soluble suppression of tumourigenicity 2, a marker of inflammation. The robust relationship between biomarkers’ values and trends and the HF prognosis implies that serially monitoring these biomarkers may help inform medication adjustments and improve patient prognosis.1
B-type natriuretic peptide (BNP) and N-terminal pro-brain natriuretic peptide (NT-proBNP) have been most examined for their usefulness for guiding therapy. Several studies have examined whether NP-guided treatment enhances the titration of medical therapy, reduces NP values and improves symptoms and prognosis (Table 1).6–12 The earliest study was STARS-BNP.6 In this randomized controlled trial, the prognostic impact of BNP-guided intervention was examined in 220 patients with chronic HF with ejection fraction (EF) <45% who were receiving optimal medical therapy with angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers and beta-blockers. The BNP-guided group was treated to reduce BNP levels to <100 pg/mL, while the BNP-unguided group received standard therapy, and BNP levels were not measured. The BNP-guided group had significantly lower rates of death related to HF or unplanned hospital stays for HF than the BNP-unguided group. While all-cause mortality and all-cause hospitalizations did not differ between the two groups, HF hospitalizations were significantly lower in the BNP-guided group.6

The PROTECT study examined the impact of NP-guided therapy on cardiac function and quality of life.7 The study randomized 151 patients with HFrEF to an NT-proBNP-guided or -unguided group. In the NP-guided group, NT-proBNP values were measured every 3 months, and patients received intensified pharmacotherapy when levels reached >1,000 pg/mL. At the end of the study, the NT-proBNP-guided group was more frequently treated with aldosterone antagonists and less frequently treated with loop diuretics than the unguided group. As a result, the primary endpoint of cardiovascular events was significantly lower, and improvement in quality of life was significantly greater in the NT-proBNP-guided group versus the unguided group. In addition, echocardiographic findings showed greater improvement in left ventricular EF, end-systolic volume fraction and end-diastolic volume fraction in the NT-proBNP-guided group.7
The unique BATTLESCARRED study randomized 364 patients with chronic HF to NT-proBNP-guided therapy, clinically guided therapy or usual care by a family physician.8 In the NT-proBNP-guided group, drug therapy was adjusted when NT-proBNP value was >150 pmol/L (around 1,300 pg/mL). One-year mortality was significantly lower in the NT-proBNP-guided and clinically guided groups than in the usual care group (9.1% versus 9.1% versus 18.9%, respectively). Three-year mortality was significantly lower only in the NT-proBNP-guided group (15.5% versus 30.9% versus 31.3%, respectively) in patients under 75 years of age. In contrast, there was no benefit in patients over 75 years of age, suggesting that NT-proBNP-guided therapy may not be helpful in the elderly.8
Similar results were observed in another study, where patients were stratified according to age below and above 75 years. The TIME-CHF study randomized 499 patients with HFrEF to NT-proBNP-guided therapy or usual care.9 In the NP-guided group, target NT-proBNP was <400 pg/mL for patients <75 years of age and <800 pg/mL for patients ≥75 years of age. Although the pharmacotherapy was more aggressively adjusted in the NP-guided therapy group, the primary endpoint of avoidance of all-cause hospitalization at 18 months did not differ between the groups. In addition, quality of life improved significantly in both groups at 12 months, with no difference between the groups. In patients <75 years old, NT-proBNP-guided treatment was associated with lower rates of hospitalization for HF than usual care. However, this finding was not observed in patients ≥75 years old; there was no difference between
the groups.9
The PRIMA study examined the effects of NP-guided therapy with individualized target NT-proBNP values.10 In 345 patients with decompensated HF, the lowest NT-proBNP value at discharge or 2 weeks after discharge was set as the target value. Patients who exceeded this target by >10% and ≥850 pg/mL were considered ‘off-target’, and treatment was intensified. The primary endpoint of hospitalization-avoided survival days was not different between the groups (within the target versus off-target). The study reported no difference between the groups in mortality, cardiovascular hospitalizations or the number of unscheduled visits to hospital.10
Based on the results of these randomized trials, a meta-analysis reported that NP-guided therapy was superior to unguided treatment in patients younger than 75 years of age.11 However, no benefit was observed in patients aged over 75 years. Nevertheless, the studies included in this analysis were relatively small and lacked uniformity in target BNP levels and adjustment of medical therapy.
In light of these issues, the GUIDE-IT trial was designed to include 1,100 patients with HFrEF to determine the usefulness of NT-proBNP-guided therapy with a target level of 1,000 pg/mL.12 The primary endpoint was the composite of cardiovascular death and HF hospitalization. After 894 patients had been randomized, the study was stopped early due to an interim analysis suggesting no significant difference in outcomes between the guided and unguided treatment groups. At 15 months of follow-up, the primary outcome occurred in 37% of each group. There were no differences between the groups in cardiovascular death, all-cause mortality or HF hospitalizations. Notably, the NT-proBNP-guided group received higher doses of HF medications and more frequently visited the hospital for treatment, but there was no difference in the final drug therapy. There was no difference in NT-proBNP levels or the rate of achieving ≤1,000 pg/mL between the groups (31% at 90 days). NT-proBNP ≤1,000 pg/mL at 90 days was associated with a lower incidence of all-cause and cardiovascular mortality and hospitalization for HF. The GUIDE-IT trial showed that, with adequate medical therapy, the unguided group could be expected to have the same NT-proBNP reduction and prognosis as the guided group.12
Natriuretic peptide-guided therapy in heart failure with preserved ejection fraction
HFpEF usually occurs in older patients with multiple comorbidities, making it difficult for clinicians to interpret signs and symptoms of HF. Thus, an NP-guided strategy could provide an objective method to titrate HF treatment. Many studies have been carried out in patients with HFrEF, but data on HFpEF are scarce. Hence, the effect of NP-guided therapy in HFpEF has been poorly studied.
Although NP may be helpful in guiding therapy in patients with HFrEF, the evidence for benefit in HFpEF is less compelling. Among the few studies, there is only one randomized clinical trial and most data come from meta-analyses. Maeder et al. studied 123 patients with HFpEF (EF >45%) included in the TIME-CHF trial, who were compared with 499 patients with HFrEF (EF ≤45%).13 The inclusion criteria were chronic HF, age ≥60 years, New York Heart Association (NYHA) class ≥II, HF hospitalization within the last year, and age-adjusted NT-proBNP levels (>400 pg/mL in those aged 60–74 years or >800 pg/mL in those ≥75 years). Patients were randomized to standard medical therapy, titrated to reduce symptoms to NYHA class ≤II or to reduce NT-proBNP below the inclusion threshold (age-adjusted). Among patients with HFpEF, NT-proBNP reduction and symptom relief were similar in the symptom-guided and NT-proBNP-guided groups, despite more aggressive treatment in the latter group. In contrast to patients with HFrEF, patients with HFpEF did not benefit from this strategy. In fact, NP-guided therapy tended to worsen 18-month outcomes in patients with HFpEF. Survival free of any hospitalization, the primary endpoint, was worse in patients with HFpEF compared with those with HFrEF (36% versus 41%, respectively, p=0.02). Among patients with HFpEF, hospitalization-free survival at 18 months did not significantly differ between those randomized to NT-proBNP-guided or symptom-guided therapy.13
This finding was later confirmed in an individual patient data (IPD) meta-analysis, which found that NP-guided therapy was helpful in HFrEF but not in HFpEF.14 In this analysis, comorbidities seemed to influence the response to treatment. Among patients with HFpEF, those without hypertension had worse outcomes when allocated to the NP-guided group. Conversely, patients with HFpEF with a history of renal failure fared worse on NP-guided management.14 In contrast, patients with the so-called ‘mid-range’ EF, now referred to as mildly reduced EF (HFmrEF), seem to have the same benefits with NP-guided therapy as patients with HFrEF. Using data from the TIME-CHF trial, Rickenbacher et al. demonstrated a benefit of NT-proBNP-guided therapy regarding survival free of HF hospitalization in HFrEF and HFmrEF but not in HFpEF.15
More recently, two additional meta-analyses have been published.16,17 The strengths of these meta-analyses are the large number of patients and the inclusion of data from the GUIDE-IT trial, which is the largest study assessing the NP-guided strategy. Khan et al. analysed 18 trials, with 5,116 patients, and there were no benefits with NP-guided therapy in the reduced or preserved EF groups.16 In the meta-analysis by Pufulete et al., 14 trials (five with IPD) were included.17 Regarding all-cause mortality, the NP-guided strategy benefitted patients with HFrEF (hazard ratio [HR] 0.84, 95% confidence interval [CI] 0.71–0.99) but not those with HFpEF (HR 1.33, 95% CI 0.83–2.11).17
The cost-effectiveness of NP-guided therapy has been evaluated in two studies.18,19 Mohiuddin et al. found that this strategy is potentially cost-saving in young patients with HFpEF and older patients with HFrEF, but they pointed out that more evidence is required.18 In another analysis performed in the UK, BNP-guided therapy compared with conventional care improved median survival in patients aged <75 years with HFrEF or HFpEF, with a small gain in quality-adjusted life-years (5.68 versus 5.02) but higher lifetime costs (£64,777 versus £58,139).19
Table 2 summarizes the main studies of NP-guided therapy in HFpEF.13–19 Taken together, the available evidence suggests that patients with HFpEF do not benefit from NP-guided therapy. In addition, using NP in the inclusion criteria for clinical trials in HFpEF has been a matter of debate, as the effects of the medications in these trials were independent of NP levels. For example, in the I-PRESERVE and TOPCAT trials, the effects of irbesartan or spironolactone were reduced or absent in patients with high NP values at baseline.20–22 Similarly, in the PARAGON-HF trial, no treatment effects of sacubitril/valsartan differed according to baseline NP levels.23
A possible explanation for the unsuccessful results of NP-guided management in HFpEF could be that drugs with proven benefits in HFrEF are not equally effective in patients with HFpEF,1 suggesting that intensifying the existing drug treatment will add little or no benefit. New studies should include treatment with SGLT2is, the only drugs with proven benefits in HFpEF so far.24

Natriuretic peptide-guided therapy in acute heart failure
In patients with acute HF, BNP and NT-proBNP are useful for diagnosis and risk stratification. High NP levels on admission predict poor prognosis, and a decrease in NPs with in-hospital treatment is associated with improved outcomes.25 The PRIMA II trial evaluated whether NT-proBNP-guided therapy, which aimed to reduce NT-proBNP by >30% at discharge, improves outcomes compared with unguided therapy, in patients with acute decompensated HF.26 A total of 405 patients were randomized, including those with HFrEF and HFpEF. The primary endpoints were 1) a composite of all-cause mortality and HF readmissions in 180 days, and 2) the number of days alive out of the hospital in 180 days. The reduction of NT-proBNP by >30% at discharge was more frequently observed in the NT-proBNP-guided group (80% versus 64%, p=0.001). However, the incidence of the composite endpoint was not different between the groups (all-cause mortality and HF readmission: 36% versus 36%, p=0.99; median out-of-hospital survival: 178 versus 179 days, p=0.39, in guided and unguided groups, respectively). Secondary endpoints were all-cause mortality within 180 days, HF readmissions within 180 days, and a composite of all-cause mortality and HF readmissions within 90 days. None of them was improved with NP-guided therapy.26
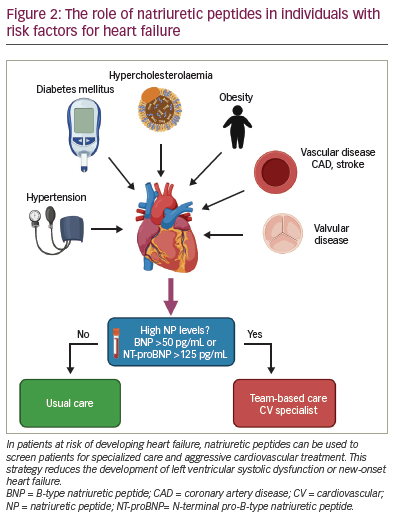
Natriuretic peptide-guided therapy in the prevention of heart failure
Controlling cardiovascular risk factors is useful in preventing cardiac disorders, including HF. A few studies have shown that NP can identify patients at risk for HF, and NP-guided therapy may reduce the incidence of HF in this scenario.27,28 In the STOP-HF trial, 1,341 participants with cardiovascular risk factors were randomized to usual primary care (control group) or to an intervention group, screening with BNP testing.27 Patients in the intervention group with BNP ≥50 pg/mL were referred for echocardiography and collaborative care between the primary physician and a specialist cardiovascular service. Left ventricular dysfunction with or without HF was reduced in the BNP-guided group versus the control group (5.3% versus 8.7%, p=0.003). Additionally, emergency cardiovascular hospitalizations were 40% less frequent in the intervention group (p=0.002).27
The PONTIAC I study randomized 300 patients with type 2 diabetes and NT-proBNP >125 pg/mL, but without heart diseases, to usual care or ‘intensified care’.28 Patients in the usual care group were managed at four diabetes care units and the intensified group was additionally managed at a cardiac outpatient clinic to up-titrate renin–angiotensin system antagonists and beta-blockers. A significant reduction in the primary endpoint (death or hospitalization due to cardiac disease after 2 years) was observed in the intensified group (p=0.044).28 The on-going study PONTIAC II, was designed to confirm these findings in a larger number of patients.29 Based on these studies, the recently published American Heart Association/American College of Cardiology/Heart Failure Society of America HF Guideline endorses the use of an NP screening strategy to prevent HF in high-risk patients.30 Figure 2 summarizes this strategy.
Conclusions
HF is a prevalent and complex syndrome, and all efforts should be made to improve outcomes. History and physical examination are the mainstay of medicine, but have limitations. Biomarkers are useful tools that complement the information obtained by clinical examination. NPs are the gold-standard biomarkers for diagnosing and prognosticating HF. However, there are conflicting data on the utility of NP for guiding therapy in HF. In HFrEF, NP-guided therapy reduces hospitalization and possibly mortality in patients aged <75 years. However, current data do not support the use of this strategy in patients with HFpEF or in hospitalized patients. In addition, the cost of measuring NP at every visit needs to be taken into account, as the cost-effectiveness of this strategy is not clear. Of note, reduced NP levels are associated with better outcomes in all scenarios, whether guided clinically or by NPs.
In patients at risk for developing HF, NP-based screening followed by specialized cardiovascular care can help prevent left ventricular dysfunction or new-onset HF. Finally, we would like to point out that, regardless of measuring NP, all medications used in treating HF need to be up-titrated, as recommended by HF guidelines.