Background: Obesity-related cardiac remodelling may be reflected through electrocardiogram (ECG) changes. Based on this premise, we hypothesised that an artificial intelligence (AI)-ECG model could be trained to predict body mass index (BMI), and that the difference between AI-ECG predicted BMI and measured BMI (delta BMI) would be a marker of cardiometabolic health. Additionally, we sought to understand the underlying biological mechanisms contributing to the AI-ECG-derived delta BMI.
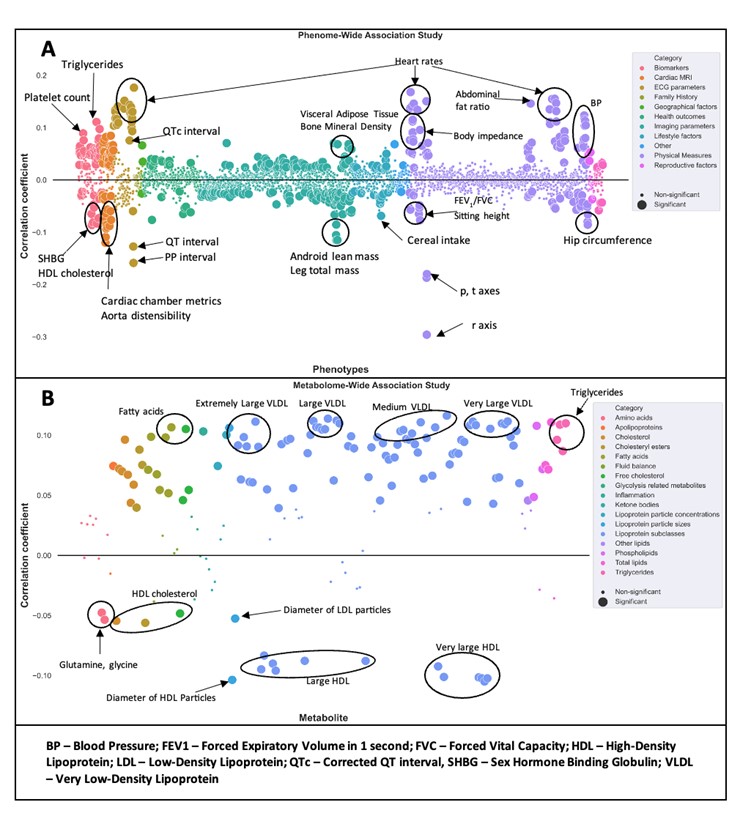
Methods and results: We developed an AI-ECG model using a cohort of 512,950 ECGs from 114,415 patients from Beth Israel Hospital Deaconess Medical Center in Boston to predict their BMI. The model’s mean absolute error was 4.09 (95% CI: 4.03–4.12) and the model’s correlation coefficient was 0.64. The model was externally validated using the UK Biobank (UKB) 12-lead ECGs from 42,386 patients. The mean absolute error was 3.92 (95% CI: 3.87–3.97) and the correlation coefficient was 0.61. Using the delta BMI values for the UKB cohort corrected for measured BMI, age, and sex, we performed Cox regression and a phenome-wide association study (PheWAS). A unit increase in the standard deviation of delta BMI was associated with an 18% increase in the risk of future hypertension (HR 1.18, 95% CI: 1.12–1.24). A PheWAS against 3,145 phenotypes revealed significant positive associations with heart rate, blood pressure, QTc interval, blood biomarkers (triglycerides, platelet count), visceral adiposity, abdominal fat ratio, and body impedance, and negative associations with cardiac chamber volumes, android lean mass and hip circumference. (Figure 1A) A metabolome-wide association study revealed significant positive associations with fatty acids, VLDL particles, and triglycerides, and negative associations with HDL particles, glutamine, and glycine (Figure 1B). A genome-wide association study of the adjusted delta BMI identified nearly significant associations with DNAH10 and CCDC92, both of which have putative roles in adipogenesis.
Conclusion: Our study demonstrates that an AI-ECG model can accurately predict body mass index. The model achieved very good performance and was successfully validated using the UK Biobank cohort. The AI-ECG-derived delta BMI captures significant associations with future hypertension, cardiac and metabolic phenotypes, and biologically plausible metabolites that are additive to measured BMI, as well as nearly significant associations with genes linked to adipogenesis. AI-ECG-derived delta BMI may be used to identify subjects at increased risk of cardiometabolic disease. ❑
Figure 1: Pacing threshold vs referenced local impedance in Stablepoint patients