Background: The spatial resolution of a mapping catheter is determined by factors such as the quantity of electrodes, their inter-electrode spacing, and the various configurations in which they are utilized. These factors impact the interpretation of wavefront dynamics during cardiac arrhythmias. Virtual patient models incorporating simulated arrhythmias offer an ideal dataset for evaluating the spatial resolution requirements, given that the precise propagation of high-resolution wavefronts is known from the high-resolution simulated data. We aimed to use a virtual patient cohort with different substrate heterogeneities and electrode set-ups to investigate the spatial resolution requirements for assessing atrial fibrillation (AF) wavefront patterns.
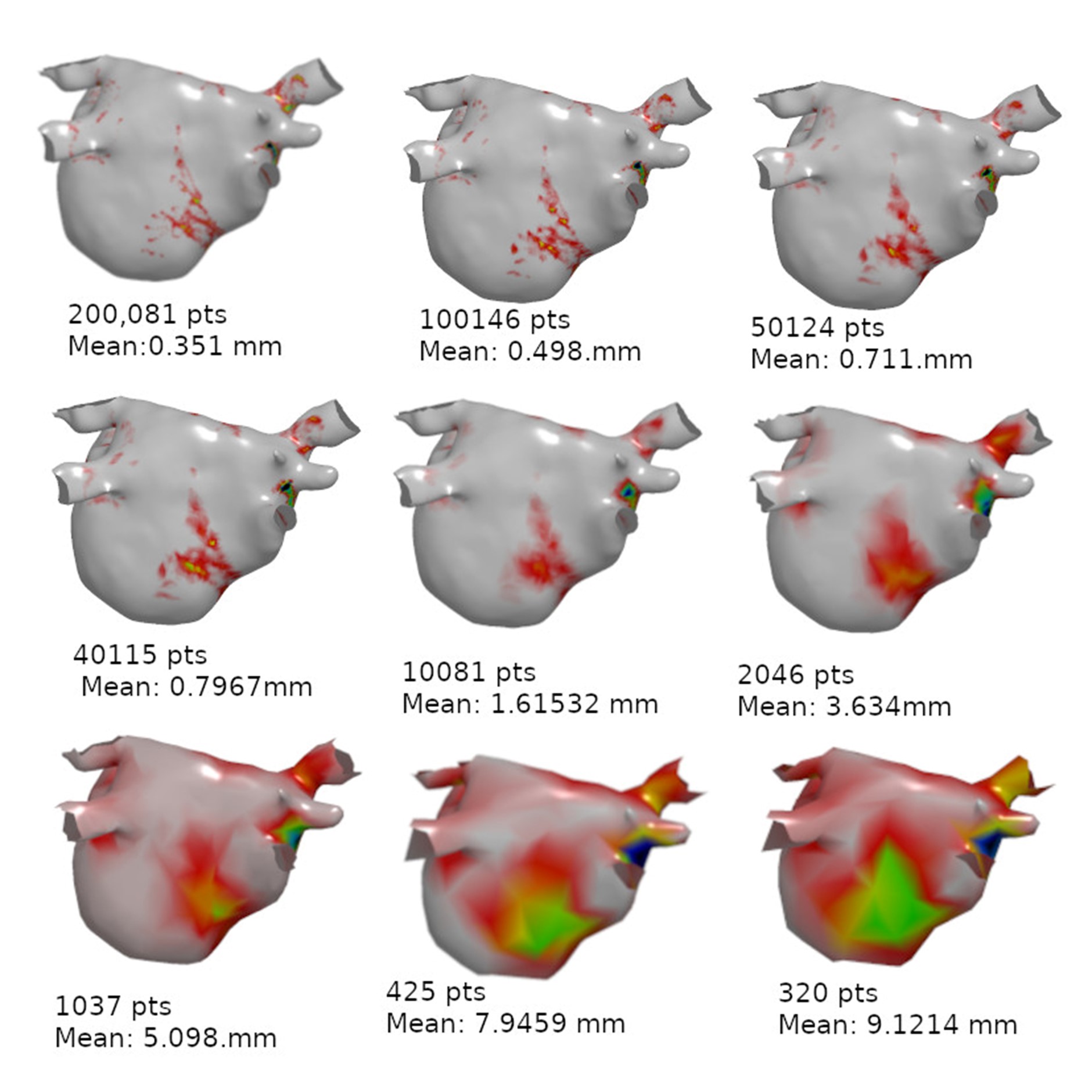
Methods: An AF model was developed where wavefront activity included areas of rotation, wavefront break-up, and focal activity. Specifically, left atrial meshes were constructed from segmented late-gadolinium enhancement MRI data, with the simulation mesh consisting of approximately 200,000 points. This high-resolution mesh served as the baseline model for subsequent down sampling and phase singularity (PS) point calculations. The purpose of these calculations was to derive a visual representation of the re-entry patterns and areas of wavefront break-up associated with the arrhythmia. The downsampling process and PS calculation were iteratively performed on each downsampled mesh until the identification of new false PS points or until PS points obtained on the high-resolution mesh were no longer identified in the downsampled mesh (missing detections).
Results: Downsampling the meshes affected the propagation of the wavefront, resulting in larger regions with decreased precision in the localization of PS points. This is visualized in Figure 1, which shows an example of how spatial resolution affects the visual interpretation of AF. We found that the critical resolution for the identification of areas of re-entry during AF is 320–350 recording points across the left atrium, corresponding to an average inter-electrode distance of 8.0–9.1mm.
Conclusions: Careful consideration of the spatial resolution of recordings is of utmost importance in the interpretation of human AF data, as it plays a substantial role in accurately understanding the underlying AF mechanism. The utilization of virtual patient models provides an additional perspective on these and other factors, thereby presenting a significant opportunity to enhance the interpretation of arrhythmias. ❑
Figure 1: PS comparison between high resolution mesh and downsampled meshes, below each model is the number of points and the mean edge length