Background: The limitations of bipolar electrograms (EGM) due to catheter orientation are well described. Omnipolar electrograms may be able to accurately identify substrate characteristics as they are not affected by directionality.
Objectives: To investigate the difference in voltage maps between omnipolar and bipolar electrograms in human atrial flutter.
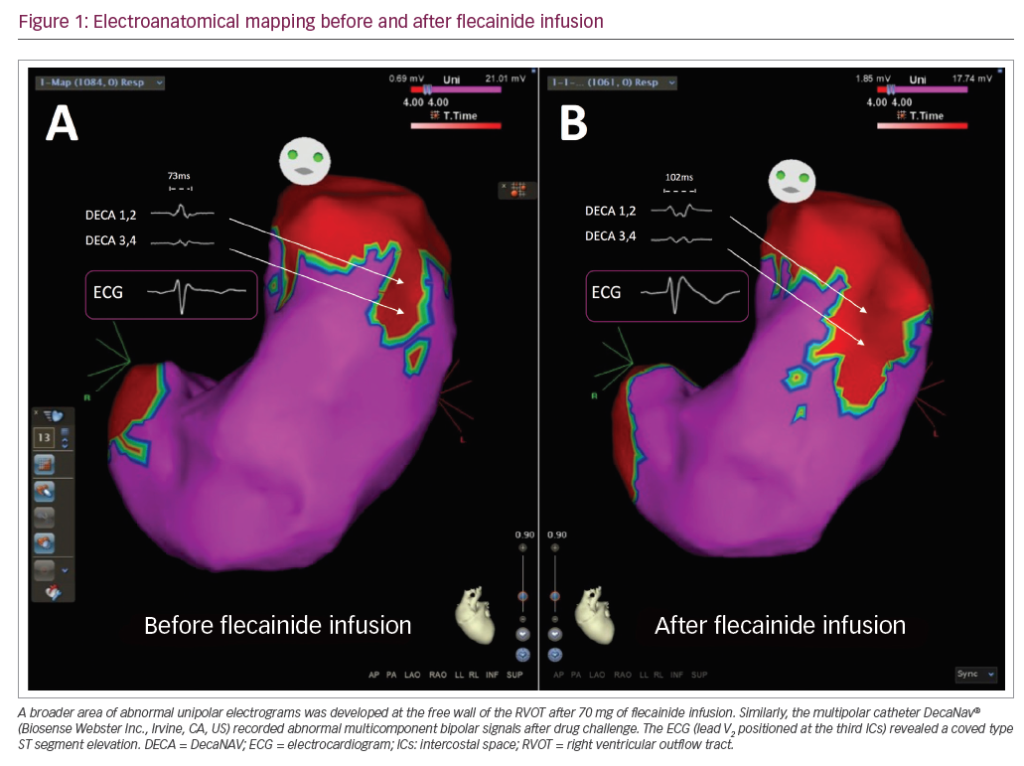
Methods: We recruited 15 patients with typical (clockwise or counterclockwise) persistent atrial flutter (AFL). All patients had bipolar (BP) voltage maps created during their clinical procedure. Omnipolar (OP) maps were derived from bipolar EGMs. Voltage maps were created using the traditional thresholds for scar and healthy tissue (dense scar <0.1 mV, 0.1–0.5 mV for scar border and >0.5 mV for healthy tissue). The 10-second segments of AFL were recorded in different areas within the RA. The HD Grid was held flat against the myocardial surface model and only points within 5 mm from the geometry were used for this analysis. Each recorded segment was analysed after a steady state of at least 8 atrial beats. We created beat-to-beat correlation curves for each segment and only highly correlating (Pearson’s r >0.7) segments were used for this analysis to ensure good contact and reproducibility (Figure 1A). OP and the maximum recorded BP voltage on either the vertical or horizontal direction (across or along the HD Grid electrodes) were compared in terms of beat-to-beat consistency and overall voltage recorded. Full BP and OP voltage maps were also created and then compared offline using area of scar projected on the geometry RA model (interpolation 5 mm) (Figure 1B). The exported recorded segments were analysed offline with R.
Results: We observed a significant difference between voltage recorded with BP and OP. In all analysed recorded segments OPV mean was 0.7 mV higher than the BPV (Figure 2A). This difference was observed along all segments of the RA and persisted in areas of low voltage at a lower magnitude. OPV highly correlated (mean Pearson’s r: 0.98) with the maximum recorded BPV for each bipolar pair (Figure 2B) and was always higher (OPV 2.48 ± 2.89 mV vs BPV 1.78 ± 2.25 mV; p<0.001). OPV was more consistent on a beat-to-beat basis than BPV (coefficient of variation: OTV 0.34 ± 0.2 vs BPV 0.45 ± 0.21; p<0.001). Average OP scar area was 37% less compared with the BP scar area as projected on the surface of the RA model (interpolation 5 mm) (p<0.001) (Figure 2C).
Discussion: The ability of OP EGM to always record maximum voltage in a given location irrespective of direction increases the sensitivity of detecting healthy tissue, especially in low-voltage border zones of scar. Beat-by-beat consistency in EGM recorded increases confidence in the fidelity of the voltage maps created. OP mapping has the potential to improve detection of scar border zones, which may serve as isthmuses for arrhythmia maintenance and therefore improve ablation accuracy and outcomes.