Bicuspid aortic valve (BAV) represents the most common congenital cardiac anomaly, with a prevalence ranging between 1% and 2% in the general population.1 BAV is known to be associated with dilation and dissection of the ascending aorta, and the significantly higher shear forces seem to have a pivotal role on the development of such complications.2 Nowadays, patients with BAV are frequently encountered in clinical practice, presenting coronary artery disease or other comorbidities, due to the increasing survival age of the congenital heart disease population.3 While some recent investigations have characterised aortic flow patterns as well as the time-averaged wall shear stress (TAWSS),4–5 the aortic arch flow pattern in patients with BAV with a coexisting ostial/mid-shaft left main (LM) stenosis have not been analysed yet. We describe the TAWSS in a patient with normally functioning BAV and significant ostial/mid-shaft LM stenosis before and after LM stenting using computational fluid dynamic analysis (CFD). Informed consent was obtained from the patient and the approval by the local ethics committee was waived due to the type of study.
Case report
A 47-year-old female patient with normally functioning BAV and fusion of right and non-coronary cusps was investigated for unstable angina. Proximal arteries and aortic arch were reconstructed using coronary computed tomography angiography with a 64-slice multi-detector computed tomography scanner (64-detector row Lightspeed VCT scanner, GE Healthcare, Milwaukee, WI, USA) to define the morphology and degree of dilation of ascending aorta.
The acquired images were then segmented to reconstruct the vascular anatomy in 3D. Coronary artery stenosis and minimal lumen area were calculated considering the reconstructed coronary artery model. Specifically, the severity of the LM stenosis was computed as 100% minus the percentage of minimal lumen area to the reference lumen area. Blood was modelled as a laminar non-Newtonian and incompressible fluid. Reconstruction and CFD analysis of coronary artery TAWSS were trunked to the proximal segment of the vessels. The aortic wall was assumed to be elastic with a radial dilation of the proximal aorta of 8% (physiological value around 10%) and a total arterial compliance of 1.75 mL/mmHg (physiological value 1.84 ± 0.76 mL/mmHg).3 To estimate the patient-specific flow rate, the patient-specific stroke volume was calculated from the difference between the end-diastolic and end-systolic volumes, and then combined with the measured heart rate to obtain their time-averaged flow rate. Then the calculated velocity was applied as an inlet boundary condition at the left ventricular outflow tract.
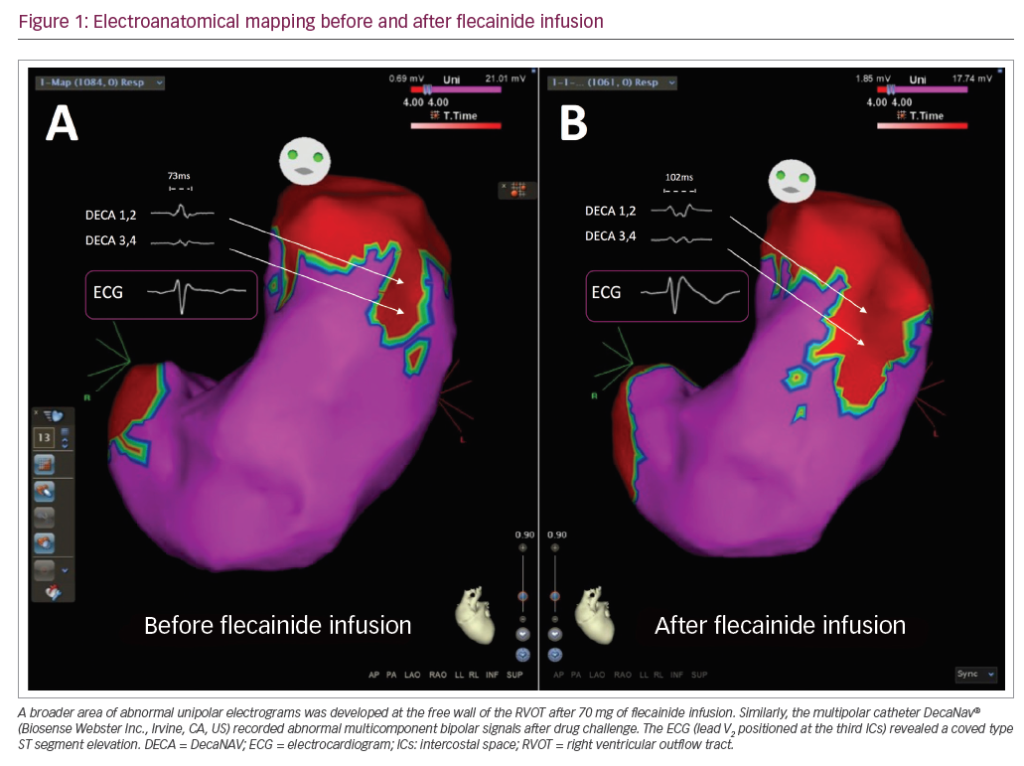
Stress mapping of the ascending aorta before LM stenting showed a mean TAWSS of 9.4 Pa, and was associated with higher TAWSS values at the site of LM stenosis (Figure 1A). The LM lesion was treated by stent implantation treating the target lesion with an Orsiro (Biotronik, Berlin, Germany) 4.0 × 12 mm at 18 atm. Stent implantation was preceded by pre-dilation with non-compliant Euphora (Medtronic Inc., Santa Rosa, CA, USA) balloon 3.0 × 12 mm at 16 atm and followed by an over-dilation with 4.5 × 12 mm non-compliant Euphora balloon at 20 atm. The reconstructed post-procedural model revealed a decrease of the mean ascending aorta TAWSS to 5.6 Pa.

Discussion
Our case demonstrated that the treatment of a LM lesion in our patient with BAV improved the TAWSS in the ascending aorta, potentially protecting the ascending aorta from the well-known complications of BAV. Although the association between BAV and LM disease remains very rare in young subjects, the increasing percentage of patients with congenital heart disease reaching middle age and older makes the association between BAV and coronary artery disease more likely to be clinically relevant.3
Using 4D flow-sensitive magnetic resonance imaging, Barker et al. demonstrated an increased and asymmetric wall shear stress (WSS) at the aorta wall related to ascending aortic flow jet patterns, which were influenced by the BAV fusion pattern.7 Similarly, Guzzardi et al. observed that regions of increased WSS correlated with extracellular matrix dysregulation and elastic fibre degeneration in the ascending aorta of patients with BAV, suggesting that valve-related haemodynamics may be a contributing factor in the development of aortopathy.8
Using CFD analysis in LM disease, our group have already demonstrated that not only a concomitant LM lesion but also the type of stenting significantly modifies the WSS over the ascending aorta.5 Extending the stent coverage up to the ostium, when the ostial region is not diseased, might induce unfavourable alterations of flow, not only at the level of the LM lesion and ostium, but also in the ascending aorta and aortic arch, potentially predisposing the aortic wall to long-term damage. In the case of BAV, which already perturbates the aortic arch flow, we hypothesised that the increased thickness of the vessel at the atherosclerotic lesion site may create an additional rigidity point in the aortic wall at the LM site, further worsening the aortic arch flow. This condition, as suggested in the case presented here, can be ameliorated by LM stenting, especially in middle-aged patients where BAV and coronary atherosclerosis can be more frequently associated.
Conclusion
The treatment of an LM lesion in patients with BAV has the potential to improve TAWSS in the ascending aorta, protecting the ascending aorta from the well-known complications of BAV.