Background: Catheter ablation is an effective therapy for ventricular tachycardia (VT) secondary to ischaemic heart disease (IHD), but its wider adoption is limited by procedure complexity and safety. Pre-procedural planning with cardiac computer tomography (CT) or magnetic resonance (MR) and their integration into electro-anatomical mapping (EAM) during ablation have sought to address some of the associated challenges. The aim of this study was to investigate the impact of pre-procedural cardiac CT or MR on VT catheter ablation outcomes in patients with IHD.
Methods: Fifty-five patients with IHD who underwent VT substrate ablation in our centre from 2013–2019 were included in this retrospective analysis. Baseline characteristics and procedure details were compared between patients who underwent 3D-reconstructed imaging-guided ablation (n=25, 88% cardiac CT, 12% MR) and those with no imaging (n=30). Technical, immediate clinical and longer-term outcomes were then explored.
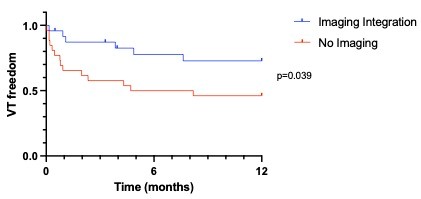
Results: Fluoroscopy dose reduced over time in procedures with imaging integration (r=-0.51, p=0.01), but not in those without (r=-0.27, p=0.22). There was no difference in procedure time, acute complication rate or VT inducibility after ablation between the 2 groups. VT freedom after 12 months was higher in imaging-guided ablations compared with no pre-procedural imaging (log-rank 0.039) (Figure 1). After excluding deaths within 12 months, 42% of patients with no pre-ablation imaging had a repeat procedure during this timeframe, while none in the imagingguided group did.
Conclusion: Integration of cardiac CT or MR with electro-anatomical mapping is associated with a higher rate of VT freedom. With increasing experience, use of imaging reduces the dose of radiation required during substrate ablation. ❑
Figure 1