Introduction: Contemporary imaging methods allow to assess structural alterations implicated in initiation and maintenance of AF. It is thought that left atrial wall thickness (LAWT) increases in the presence of AF and may further promote its perpetuation. Tissue thickness may also be important to the success and safety of AF ablation to create transmural lesions without causing collateral damage. Different methods for quantifying local LAWT exist. An understanding of quantitative differences between estimation methods is relevant if LAWT-guided ablation strategies are pursued.
Methods: Patients with AF and controls without AF but with clinical indication for cardiac CT were recruited. The study received a favourable opinion from a national REC (ref 15/LO/1803). Prospective, ECG gated CCTA were acquired and best diastolic sequence identified. Two separate segmentation pipelines and LAWT calculation methods were employed:
- A semi-automated custom-made workflow using an eikonal-based calculation (“KCL”): CT images were segmented with custom-made Python scripts to extract LA myocardium based on Hounsfield unit and crop the mitral annulus with a sphere (Seg3D2). Pulmonary veins and LAA were cropped using CEMRG app. The LA body segmentations were used to generate tetrahedral meshes (CGAL) for identification and extraction of endocardial and epicardial surfaces (Meshtool). Using the cardiac arrhythmia research package (CARP), vertices on the epicardial surfaces were activated simultaneously with the wavefront having a constant isotropic conduction velocity of 1 mm/s. LAWT was then estimated as the wavefront arrival time at the endocardium.
- An automated proprietary LAWT analyzing tool integrated in ADAS3DTM software (V2.11.1-beta.10): Following CT integration, endocardial and epicardial delineation is fully automated and generates a 3D endo- and epicardial surface mesh, followed by manual review and adjustment of the model as appropriate. LAWT computation is based on the distance of each point on the endocardial surface of the corresponding closest point on the epicardial surface. PVs, LAA and mitral valves are cropped manually.
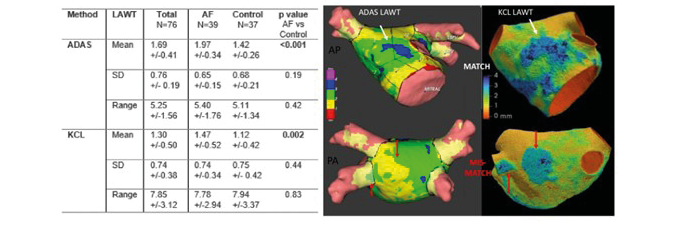
Results of mean ± SD of LAWT of the LA body were compared between methods for the total population and separately for AF and control cohorts. Statistical significance was set at α 0.05.
Results: Forty-two patients with AF (64.3% male, age 64.6 ± 10.2, CHA2DS2-VASc 2.48 ± 1.5, 69.0% paroxysmal AF, 31% persistent AF, LVEF 57.9 ± 10.5%) and 37 controls (64.9% male, age 56.6 ± 7.2, CHA2DS2-VASc 1.54 ± 1, LVEF 60.4 ± 4.9%) were recruited. A total of 76 CTs (39 AF, 37 control,) were analyzed. Mean LAWT between the 2 methods showed moderate, statistically significant correlation (r 0.499, p<0.001) and mean difference of 0.39 mm (p.001). LAWT was higher using ADAS3D in all groups (total, AF, control). Both methods identified a statistically significant increase in LAWT in patients with AF when compared to controls. There was no significant difference in standard deviation between estimation methods.
Conclusions: LAWT assessment using automated nearest point LAWT estimation or semi-automated eikonal-based estimation methods yield moderate, statistically significant correlation, with mean difference in the sub-millimetre range. Even though statistically significant, for clinical ablation procedures this difference is likely to be of negligible relevance. Local expertise and available software may determine the preferred approach for LAWT estimation. ❑
Figure 1: LAWT (mm) mean, SD and range calculated by Adas3D and KCL method with exemplary 3D models