Background: Direct current electrical cardioversion (DCCV) is utilized for managing patients with symptomatic persistent atrial fibrillation (AF) as part of a rhythm-control strategy. Rates of acute conversion and maintenance of sinus rhythm (SR) following DCCV improve with concomitant use of anti-arrhythmic drugs (AAD) such as amiodarone, which has the greatest efficacy amongst various agents, albeit with a considerable side-effect profile. Ranolazine, primarily used as an anti-anginal, has demonstrated value as an effective AAD in AF and works synergistically with class III agents. This audit aimed to evaluate freedom from persistent AF at 1 year following DCCV in patients treated with a class III AAD, ranolazine or a combination of the two.
Methods: DCCV lists between June 2020 and February 2022 at a single tertiary cardiology centre were reviewed retrospectively. Patients undergoing DCCV on treatment with either a class III AAD (amiodarone or dronedarone), ranolazine (dosage range: 375–750 mg BD) or a combination of the two, and with a documented 1-year (range: 9–15 months) follow-up were included. Patients who underwent AF ablation during the follow-up period having maintained SR up to that point were excluded. Acute DCCV success and maintenance of SR at 1-year follow-up were recorded.
Results: Patient characteristics: 350 patients underwent DCCV during the study period, of whom 102 (29.1%) were on an anti-arrhythmic drug. After exclusions, 78 patients (mean age 67 ± 11.8 years, 82.3% male) were included. Baseline characteristics for patients in the treatment groups were as follows:
- amiodarone monotherapy: n=30, 65 ± 14.5 years, 83.3% male
- dronedarone monotherapy: n=23, 71 ± 9.1 years, 87.0% % male
- ranolazine monotherapy: n=11, 63 ± 12.2 years, 90.9% male
- ranolazine and class III AAD: n=14, 69 ± 8.3 years, 64.2% male
Acute outcome: the proportion of patients achieving SR acutely post-DCCV for the 4 groups was as follows:
- amiodarone monotherapy: 27/30 (90.0%)
- dronedarone monotherapy: 21/23 (91.3%)
- ranolazine monotherapy: 10/11 (90.9%)
- combined ranolazine and class III AAD: 14/14 (100%)
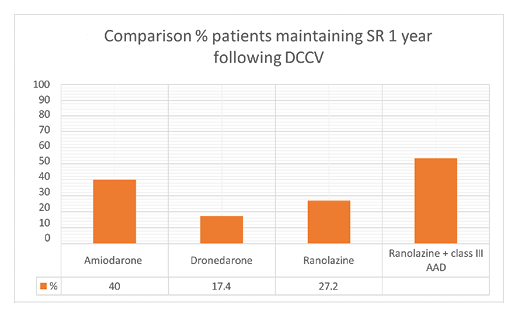
Outcome over 1-year follow-up (Figure 1): at 1-year follow-up (mean follow-up 11 ± 1.9 months – similar for all 4 groups), the proportion of patients maintaining SR was as follows:
- amiodarone monotherapy: 12/30 (40.0%)
- dronedarone monotherapy: 4/23 (17.4%)
- ranolazine monotherapy: 3/11 (27.2%)
- combined ranolazine and class III AAD: 8/14 (53.3%)
Patients taking a combination of ranolazine and a class III AAD were numerically more likely to remain in SR at 1-year follow-up than those on amiodarone or ranolazine, but this was not significant for either (P=0.34 and P=0.23, respectively). However, combination therapy was significantly more effective than dronedarone monotherapy (P=0.03).There were no significant differences between the 3 monotherapies.
Conclusion: Combining ranolazine with a Class III AAD may improve maintenance of SR at 1 year following DCCV compared with Class III AAD monotherapy. Ranolazine monotherapy also shows comparable efficacy to traditional Class III agents and could therefore be considered as an alternative agent or as synergistic therapy. Larger randomized multi-centre trials are merited to assess the efficacy and safety of these treatment strategies. ❑
Figure 1: Proportion of patients in sinus rhythm at 1-year follow-up post-direct current electrical cardioversion