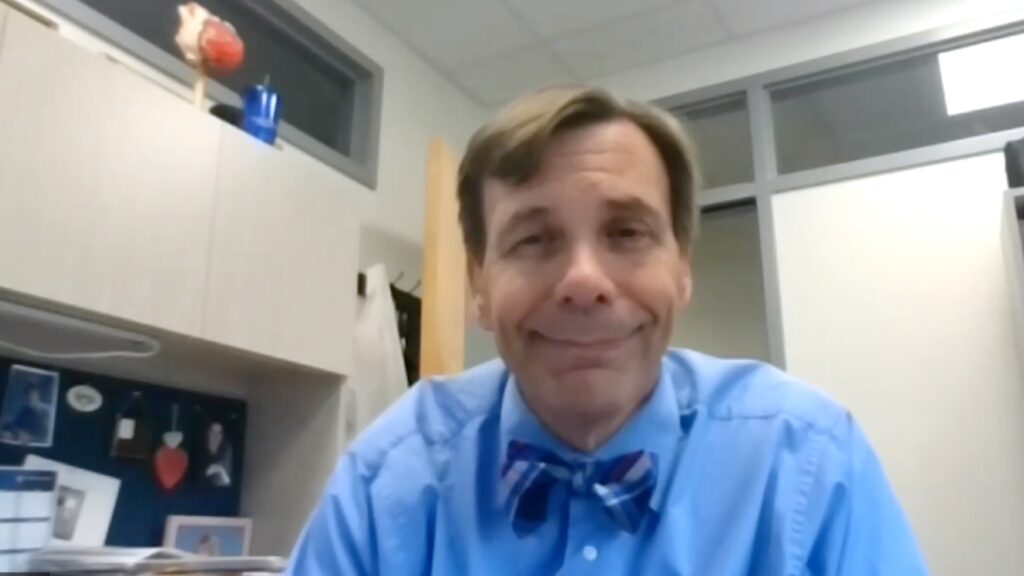
The BMAD trial investigated patients with heart failure assessed the use of the Microcor device on readmission rates. In this touchCARDIO interview, we speak with Dr John Boehmer (Penn State Milton S Hershey Medical Center, Penn State College of Medicine, Hershey, PA, USA) to discuss purpose, findings and clinical implications of the BMAD trial in patients with heart failure.
The abstract entitled ‘Impact Of Heart Failure Management Using Thoracic Fluid Monitoring From A Novel Wearable Sensor: Results Of The Benefits Of Microcor (μCor™) In Ambulatory Decompensated Heart Failure (BMAD) Trial’ (Abstract number 409-10) was presented at ACC.23 Together With WCC (ACC.23/WCC) in New Orleans, 4–6 March 2023
Questions:
- What are the current challenges in the management and monitoring of heart failure? (0:19)
- What were the aims, design and eligibility criteria of the BMAD trial? (0:52)
- What were the endpoints and how well were they achieved? (2:10)
- What will likely be the clinical impact of these findings? How will these findings be used to guide future patient management? (3:08)
Disclosures: John Boehmer is a consultant for and has received grant/research support from Zoll Medical Corporation.
Support: Interview and filming supported by Touch Medical Media. Interview conducted by Danielle Crosby.
Filmed as a highlight of ACC 2023
Access more content on Heart Failure here
Click here for Dr Boehmer’s video focussing on the MicrocorTM device for heart failure management and its comparison with other methods.
Transcript:
Hello I’m Dr John Boehmer. I’m the Medical Director of the Heart Failure Program at the Penn State Milton S Hershey Medical Center and Penn State College of Medicine.
Q: What are the current challenges in the management and monitoring of heart failure?
The challenge there is that there is a high rate of readmission following heart failure hospitalizations. Patients are often readmitted at a rate of 20% or more at 30 days and up to 40% at 90 days. So during that 90 day period, we want to find a way to monitor the patient in order to prevent them from coming back, particularly those coming back with heart failure in the same condition that they were admitted with in the first place.
Q: What were the aims, design and eligibility criteria of the BMAD trial?
The purpose was to look for the risk of heart failure hospitalization following a heart failure hospitalization. So the primary endpoint was readmission for heart failure within the 90 days following a heart failure hospitalization.
The inclusion criteria obviously dealt with people who were recently hospitalized for worsening heart failure. They also had to have another event within the prior 6 months. So we are dealing with a high risk population. Importantly, there were no ejection fraction criteria for enrollment, therefore, it had the full range of patients with heart failure. Then the exclusion criteria dealt with only things that might interfere with the device, such as a wearable AED or a subcutaneous ICD, the presence of a left ventricular assist device, another medical condition that would limit patients to a 1 year survival and sensitivity to adhesive, since this is a patch that must be worn. They had a very broad entry criteria for renal failure, which was just those anticipated to start dialysis within 90 days and those who had a recent coronary intervention. So that is all there was for inclusion criteria.
Q: What were the endpoints and how well were they achieved?
So the primary endpoint that we are reporting on is heart failure, hospitalization, and specifically the heart failure hospitalization following a recent heart failure hospitalization, also known as readmission. That was over a 90 day period.
We also looked at a combination of heart failure hospitalization, mortality and the need for emergency room visits for heart failure during that 90 day period.
Well, the primary endpoint was met with a 38% relative risk reduction in the risk of heart failure hospitalization. This corresponds to a 7% absolute risk reduction, or a number of patients needed to treat of 14 in order to have one avoid a heart failure hospitalization. In terms of the combined endpoint, it also had a 38% relative risk reduction.
Q: What will likely be the clinical impact of these findings? How will these findings be used to guide future patient management?
I think it is important that we have a broad range of tools in order to manage people with heart failure. There are clearly patients that we need to manage long term. That putting in an implantable device that we are going to monitor long term is going to be useful. However, I think we need tools for the short term risk, such as following a heart failure hospitalization, where a device such as a wearable device like the microcor can be utilized in order to manage patients during that period of high risk. If they continue to have difficulty with heart failure management, we can then move on to something that is longer term. But we need that initial monitoring in order to manage patients through this area of high risk.
Subtitles and transcript are autogenerated